Clinical Implementation of PCCT
In the last 5 years, more than 200 scientific articles have been written on photon-counting CT technology. A quick filtered PubMed search indicates roughly 60 of those are clinical by nature.
We have reviewed all of those published articles and have split our Evidence-based research report into the main clinical categories of the current publication landscape:
- Cardiovascular imaging
- Musculoskeletal imaging
- Oncology imaging
- Pediatric imaging
When we aggregated all articles, our main observations include:
- Dose reduction: 30-70% lower radiation doses demonstrated across all applications, particularly beneficial for pediatric populations 1, 2, 3, 4, 5
- Enhanced material decomposition: Enables crystal arthropathy detection and virtual non-contrast imaging without additional radiation 6, 7, 8, 9, 10
- Superior image quality: Improved spatial resolution and contrast-to-noise ratios maintained even at ultra-low doses 7, 11, 12, 13, 14
- Novel clinical capabilities: K-edge imaging for targeted contrast agents and quantitative material-specific imaging 15, 16, 17, 18
The evidence establishes PCCT as a transformative advancement in medical imaging, with proven clinical benefits across musculoskeletal, oncologic, and pediatric applications.
However, the main focus for this article is Cardiovascular Imaging.
Cardiovascular Imaging
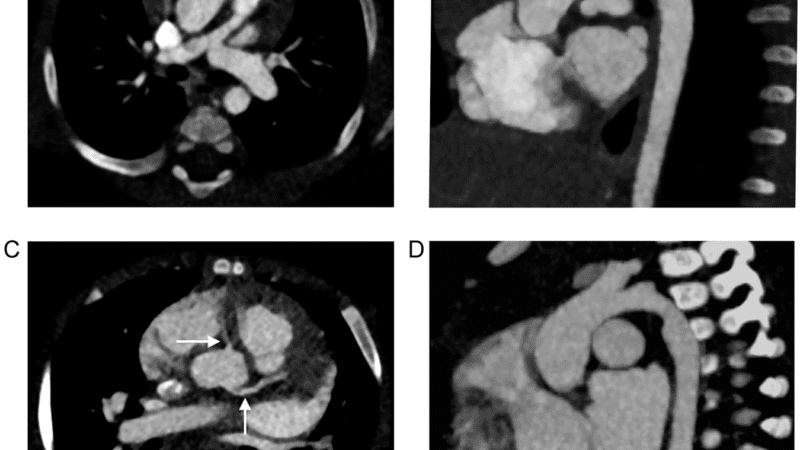
Improved coronary stent visualization and patency assessment
Recent clinical studies demonstrate improvements in coronary stent imaging with PCCT compared to conventional CT.
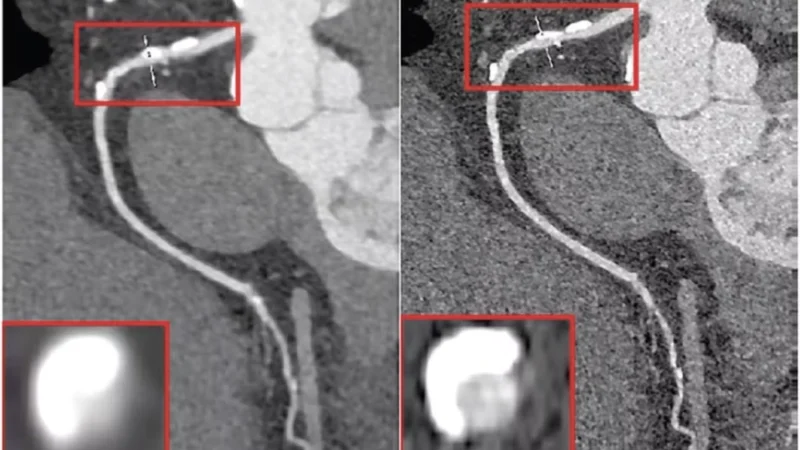
Hagar et al. (2024) conducted a prospective clinical study evaluating ultra-high-resolution PCCT for stent patency assessment in 18 patients with 44 coronary stents. The study achieved 100% sensitivity and 92.3% specificity compared to invasive coronary angiography, with only 3 of 44 stents rated as non-diagnostic. The ultra-high resolution mode with 0.2mm collimation demonstrated excellent diagnostic performance (DOI: 10.1007/s00330-023-10516-3).
Qin et al. (2024) compared standard and ultra-high-resolution protocols in 131 stents, finding that UHR images achieved 88.0% accuracy versus 78.3% for standard resolution. The study identified optimal reconstruction parameters using sharp vascular kernels (Bv72, Bv76) with 0.2mm slice thickness, significantly improving in-stent lumen visualization (DOI: 10.1007/s00330-024-10760-1).
The first in-human spectral photon counting CT study by Boccalini et al. (2022) demonstrated superior objective and subjective image quality compared to conventional dual-layer CT in 24 patients. PCCT reduced blooming artifacts (p<0.05) while achieving 25.7 mGy radiation dose versus 35.7 mGy for conventional CT, improving visualization of stent lumen and structure (DOI: 10.1097/RLI.0000000000000835, PubMed: 34711766).
Fahrni et al. (2023) provided multimodality validation showing SPCCT’s 0.25mm³ resolution versus conventional CT’s 0.625mm³ enabled superior characterization of focal suboptimal stent expansion and detection of stent gaps missed on conventional imaging (DOI: 10.1016/j.jcin.2023.07.035, PubMed: 37676223).
Enhanced plaque characterization capabilities
PCCT demonstrates advances in plaque composition analysis, vulnerable plaque detection, and differentiation between calcified and non-calcified components.
Mergen et al. (2022) conducted the first in-human quantitative plaque characterization study using ultra-high resolution PCCT in 20 patients. The technology identified 6.7% lipid-rich components versus 0.5% with standard imaging, while reducing calcified plaque proportion from 85.1% to 75.2% through reduced blooming artifacts. This improved visualization of fibrotic and lipid-rich plaque components enhances risk stratification potential (DOI: 10.3389/fcvm.2022.981012).
For vulnerable plaque detection, Dahal et al. (2024) validated PCCT against histology, demonstrating the ability to distinguish hemorrhage from fibrous cap (p=0.017), lipids (p=0.003), and necrosis (p=0.004). The study confirmed PCCT can detect rupture-prone features including thrombus, which was distinguishable from fibrosis (p=0.048) and necrotic core (p=0.017). (DOI: 10.1007/s00330-022-09155-x)
Vattay et al. (2024) analyzed 51 plaques using virtual monoenergetic imaging, finding that different energy levels (40-70 keV) substantially change plaque attenuation values and component volumes. The 70 keV reconstruction showed the lowest relative difference for calcified plaque volume assessment, demonstrating PCCT’s spectral capabilities for optimized plaque characterization (DOI: 10.1007/s00330-023-09876-7).
Si-Mohamed et al. (2022) reported a 2.3-fold higher detectability index for coronary lumen and 2.9-fold higher for non-calcified plaque compared to conventional CT, with significant reduction of blooming artifacts and enhanced diagnostic confidence confirmed by three radiologists (DOI: 10.1148/radiol.211780).
Ultra-high-resolution benefits for coronary artery disease evaluation
Ultra-high-resolution PCCT provides increased accuracy for CAD assessment, particularly in challenging patient populations.
Hagar et al. (2023) evaluated 68 high-risk patients with severe aortic valve stenosis, achieving 96% sensitivity, 84% specificity, and 88% accuracy for CAD detection. The area under ROC curve reached 0.93, with 79% of coronary segments rated as good or excellent image quality despite the challenging population. (DOI: 10.1148/radiol.223305).
Emrich et al. (2024) demonstrated that ultra-high-resolution PCCT improved stenosis quantification accuracy with mean bias of 2.3% versus 10.1% for standard resolution (P<0.001). Remarkably, 54% of patients were reclassified toward lower CAD-RADS categories, with median stenosis assessment for calcified plaques reduced from 41.5% to 26.7% (P<0.001), potentially preventing unnecessary interventions. (DOI: 10.1148/radiol.231956).
Geering et al. (2023): The ultra-high spatial resolution of 0.11×0.11mm in-plane and 0.16mm through-plane enables visualization of previously non-evaluable small vessels and reduces calcium blooming that traditionally overestimates stenosis severity. (DOI: 10.1016/j.jcct.2023.02.009)
Reduced need for invasive angiography
Multiple studies demonstrate PCCT’s potential as a gatekeeper to invasive procedures. These findings suggest PCCT could reduce healthcare costs and patient risks by decreasing unnecessary invasive procedures while maintaining appropriate referrals for intervention.
Sakai et al. (2025) analyzed 7,833 consecutive patients (3,876 PCCT vs 3,957 conventional CT), finding PCCT patients were referred less frequently to invasive angiography (9.9% vs 13.1%, P<0.001). Among those referred, the revascularization rate was higher (43.4% vs 35.5%, P=0.02), indicating improved patient selection and reduced unnecessary catheterizations. (DOI: 10.1016/j.jacc.2024.10.069).
The stent patency assessment capabilities demonstrated by Hagar et al. (2024) with 100% sensitivity and 92.3% specificity provide a non-invasive alternative to invasive angiography for stent evaluation, potentially eliminating the need for invasive assessment in many cases (DOI: 10.1007/s00330-023-10516-3).
CAD-RADS reclassification studies
PCCT consistently demonstrates reclassification of coronary stenosis severity.
An Academic Radiology (2023) study of 23 patients with 34 coronary stenoses found ultra-high-resolution PCCT decreased percent diameter stenosis by an average of 11% relative to conventional CT. This resulted in 13 of 34 stenoses being downgraded in severity category: 3 lesions from moderate to minimal, 9 from mild to minimal, and 1 from moderate to mild. (DOI: 10.1016/j.ejrad.2023.110746)
Vecsey-Nagy et al. (2025) reported ultrahigh-spatial-resolution PCCT allowed reclassification to lower disease category in 54% of patients, primarily due to reduced overestimation of stenosis from calcium blooming. This has significant implications for patient management and treatment decisions (DOI: 10.1148/radiol.241479).
The European Journal of Radiology (2023) study confirmed PCCT maintained superior accuracy across all heart rates (60-100 bpm), with improved stenosis quantification compared to standard resolution: 57.1% vs 50.0% at 60 bpm and 61.0% vs 52.4% at 100 bpm (DOI: 10.1016/j.ejrad.2023.110608).
Clinical impact summary
The evidence demonstrates PCCT’s transformative potential in cardiovascular imaging through:
- Diagnostic accuracy improvements: Sensitivity reaching 96% and specificity up to 92.3% for various applications, Springer substantially exceeding conventional CT performance.
- Clinical workflow enhancement: Non-diagnostic segments reduced to 5% versus typical 10-15% for conventional CT, Springer with 27% improvement in reader confidence. PubMed Central
- Patient outcome benefits: Reduced invasive referrals, improved risk stratification, and more accurate treatment planning through better plaque characterization and stenosis assessment.
- Technical advantages: Ultra-high spatial resolution, reduced blooming artifacts, spectral imaging capabilities, RSNA and lower radiation doses in many applications. RSNAScienceDirect
The consistent findings across multiple centers and patient populations provide robust evidence supporting PCCT implementation in cardiovascular imaging, with particular strength in complex cases involving calcified lesions, small vessels, and coronary stents.
References
- Shah KD, Zhou J, Roper J, Dhabaan A, Al-Hallaq H, Pourmorteza A, Yang X. Photon-Counting CT in Cancer Radiotherapy: Technological Advances and Clinical Benefits. ArXiv [Preprint]. 2024 Dec 4:arXiv:2410.20236v3. Update in: Phys Med Biol. 2025 May 16;70(10). doi: 10.1088/1361-6560/add4ba.
- Niehoff JH, Carmichael AF, Woeltjen MM, Boriesosdick J, Michael AE, Schmidt B, Panknin C, Flohr TG, Shahzadi I, Piechota H, Borggrefe J, Kroeger JR. Clinical Low-Dose Photon-Counting CT for the Detection of Urolithiasis: Radiation Dose Reduction Is Possible without Compromising Image Quality. Diagnostics (Basel). 2023 Jan 26;13(3):458. doi: 10.3390/diagnostics13030458.
- Lachance C, Horton J; Authors. Photon-Counting CT: High Resolution, Less Radiation: Emerging Health Technologies [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2024 Feb. Available from: https://www.ncbi.nlm.nih.gov/books/NBK602525/
- Photon-Counting Detector Computed Tomography Wu, Patricia Wanping et al. Advances in Clinical Radiology, Volume 6, Issue 1, 277 – 288. DOI: 10.1016/j.yacr.2024.05.004
- Ajay A Madhavan, Girish Bathla, John C Benson, Felix E Diehn, Alex A Nagelschneider, Vance T Lehman, High yield clinical applications for photon counting CT in neurovascular imaging, British Journal of Radiology, Volume 97, Issue 1157, May 2024, Pages 894–901, https://doi.org/10.1093/bjr/tqae058
- Photon-counting CT: Review of initial clinical results van der Bie, Judith et al. European Journal of Radiology, Volume 163, 110829. DOI: 10.1016/j.ejrad.2023.110829
- Clinical Applications of Photon-counting CT: A Review of Pioneer Studies and a Glimpse into the Future Philippe C. Douek, Sara Boccalini, Edwin H. G. Oei, David P. Cormode, Amir Pourmorteza, Loic Boussel, Salim A. Si-Mohamed, and Ricardo P. J. Budde. Radiology 2023 309:1. https://doi.org/10.1148/radiol.222432
- Filippucci E, Reginato AM, Thiele RG. Imaging of crystalline arthropathy in 2020. Best Pract Res Clin Rheumatol. 2020 Dec;34(6):101595. doi: 10.1016/j.berh.2020.101595.
- Wellenberg RHH, Hakvoort ET, Slump CH, Boomsma MF, Maas M, Streekstra GJ. Metal artifact reduction techniques in musculoskeletal CT-imaging. Eur J Radiol. 2018 Oct;107:60-69. doi: 10.1016/j.ejrad.2018.08.010.
- McCollough, C.H., Rajendran, K., Baffour, F.I. et al. Clinical applications of photon counting detector CT. Eur Radiol 33, 5309–5320 (2023). https://doi.org/10.1007/s00330-023-09596-y
- Yingyi Wu, Zheng Ye, Jie Chen, Liping Deng, Bin Song. Photon Counting CT: Technical Principles, Clinical Applications, and Future Prospects, Academic Radiology, Volume 30, Issue 10, 2023, Pages 2362-2382, ISSN 1076-6332, https://doi.org/10.1016/j.acra.2023.05.029.
- Jayasai R. Rajagopal, Faraz Farhadi, Justin Solomon, Pooyan Sahbaee, Babak Saboury, William F. Pritchard, Elizabeth C. Jones, Ehsan Samei. Comparison of Low Dose Performance of Photon-Counting and Energy Integrating CT, Academic Radiology, Volume 28, Issue 12, 2021, Pages 1754-1760, ISSN 1076-6332, https://doi.org/10.1016/j.acra.2020.07.033.
- Rajagopal JR, Farhadi F, Solomon J, Sahbaee P, Saboury B, Pritchard WF, Jones EC, Samei E. Comparison of Low Dose Performance of Photon-Counting and Energy Integrating CT. Acad Radiol. 2021 Dec;28(12):1754-1760. doi: 10.1016/j.acra.2020.07.033.
- Grunz JP, Huflage H. Photon-Counting Detector CT Applications in Musculoskeletal Radiology. Invest Radiol. 2025 Mar 1;60(3):198-204. doi: 10.1097/RLI.0000000000001108.
- https://www.spectralphotoncountingct.com/en/page/contrast-agents-k-edge-imaging
- Jost G, McDermott M, Gutjahr R, Nowak T, Schmidt B, Pietsch H. New Contrast Media for K-Edge Imaging With Photon-Counting Detector CT. Invest Radiol. 2023 Jul 1;58(7):515-522. doi: 10.1097/RLI.0000000000000978.
- Hsieh SS, Leng S, Rajendran K, Tao S, McCollough CH. Photon Counting CT: Clinical Applications and Future Developments. IEEE Trans Radiat Plasma Med Sci. 2021 Jul;5(4):441-452. doi: 10.1109/trpms.2020.3020212.
- McCollough, C.H., Rajendran, K., Baffour, F.I. et al. Clinical applications of photon counting detector CT. Eur Radiol 33, 5309–5320 (2023). https://doi.org/10.1007/s00330-023-09596-y